When will we be able to take our masks off and return to normalcy?
Our knowledge about the coronavirus and its vaccines to protect us from it are a complex and fast-evolving science. In this blog, I have endeavored to keep my discussion about it as understandable as possible. Some of the things I discuss are in reality more nuanced than what I have written here. I’ve tried to capture the essence of the ideas.
When can we stop social distancing, take our face masks off and again safely return to school, workplaces and public places to socialize, party, play, be entertained, shop, exercise and dine and drink?
It now appears the U.S. will soon have two coronavirus vaccines available. Both have completed Phase 3 trials and have filed for emergency authorization with the FDA (there are many other vaccine candidates still in Phase 3 trials). The Pfizer-BioNTech vaccine showed a 95% efficacy (94% for adults 65+) and should start limited distribution this month. The Moderna vaccine showed a 94.5% efficacy with anticipated distribution starting early next year.
The efficacy reported from the trials is the measure of what percentage of people who get the vaccine are prevented from getting sick, from becoming symptomatic. At 95% efficacy, for every 100 vaccinated people exposed to the coronavirus, 95 won’t get sick, and five will. Efficacy is measured during clinical trials. Typically, under real-world conditions when used in the general population, a vaccine’s ‘effectiveness’ tends to be lower than its efficacy.
Neither vaccine trial regularly tested volunteers to gauge asymptomatic infections, whether the vaccines prevent infection as well as the illness. That could mean that vaccinated people could still be asymptomatic carriers of Covid-19 and spread the virus to others. Medical professionals believe there is no reason to think the two vaccines won’t block transmission. It’s just that it hasn’t been measured. Also, neither trial definitely determined whether the vaccines lowered the death rate. Although fewer vaccinated volunteers in the trials got sick, those who did might have died at a high rate. It could be that the small percentage of people who don’t acquire immunity from the vaccines are the ones most prone to severe illness and death.
The answer to “when can we get back to normal?” is that the population needs to achieve ‘herd immunity’ to slow and eventually stop the virus from spreading. The concept of herd immunity is that if a sufficiently large percentage of the population, known as the ‘threshold,’ acquire immunity through prior infection or vaccination, then any individual who somehow contracts the virus is unlikely to encounter another person who is not immune and the chain of transmission stops. Once herd immunity is reached, Rt, the effective reproduction number, a measure of how fast the virus is spreading, drops to close to zero. Person-to-person spread then becomes unlikely, and everyone, the ‘herd,’ is indirectly protected, not just those immune. Herd immunity benefits those who can’t receive or sufficiently respond to a vaccine, such as people with compromised immune systems.
Many medical professionals hate the term herd immunity and prefer to call it ‘herd protection.’ That’s because the phenomenon doesn’t confer immunity to everyone from the virus — it only reduces the risk that vulnerable people will contact the pathogen.
It’s important to understand the coronavirus doesn’t magically disappear and stop infecting people when the herd immunity threshold is reached. That’s not when infections stop — it’s only when they start to slow down. It isn’t the end of the coronavirus infecting people.
Once herd immunity is achieved, each infected person will infect fewer than one other person. But the coronavirus will continue to spread, but at a continually slowing rate. If 100,000 people are infectious when herd immunity is achieved and they each infect 0.9 people, that’s still 90,000 new infections. Those 90,000 then infect 81,000 who then infect 72,900, etc., until the virus ultimately peters out and becomes endemic with only occasional, small outbreaks among nonimmune people in areas where vaccination rates are low. An analogy is that a runaway train doesn’t stop the instant the track begins to slope uphill. It just gradually comes to a stop.
There are several obstacles to reaching herd immunity. One is how long immunity will last? There isn’t enough history with infections to know how long immunity will last. Most experts feel it lasts at least six months. However, six months isn’t long enough to achieve herd immunity. People infected this year would lose immunity while the population is being vaccinated over the next year. Accordingly, as the number of people achieving immunity through vaccination or new infections increases, the number who are still immune through either earlier infection or early in the vaccination roll-out will be decreasing, making it difficult to reach the magic percentage who are immune simultaneously to achieve herd immunity.
Additionally, the threshold required for herd immunity has to be sustained to stamp out infections. This could require a lot of revaccinations if immunity is short-lived. And this assumes that the virus doesn’t mutate to a new form the vaccines don’t protect against. Scientists have already confirmed that Covid-19 did mutate from its original form to one that is more contagious. According to scientists, there is always the chance, though small, that the virus could evolve resistance to a vaccine, what researchers call “viral escape.”
Another obstacle is that the Pfizer and Moderna vaccines were only tested on adults. While severe Covid symptoms are extremely rare in infected children, they can still transmit the virus to other people. Pfizer has just obtained permission to test its vaccine in U.S. children as young as 12. Assuming the trial is successful, it is unlikely a vaccine for those age children would be available until sometime later in 2021.
That means that to achieve herd immunity, the entire population’s required percentage must be obtained among only adults. Most experts say the herd immunity threshold is 60% to 70%. Some are saying as low as 50%. So, for example, if the threshold for herd immunity is 70% of the entire population, that means that 89% of adults need to become immune to reach herd immunity assuming no children receive the vaccine.
In the chart below, I show some calculations for what percent of adults will need to become vaccinated from Covid-19 under different scenarios of vaccine effectiveness, herd immunity thresholds, and the most optimistic prediction of what percent of adults will get the vaccine.
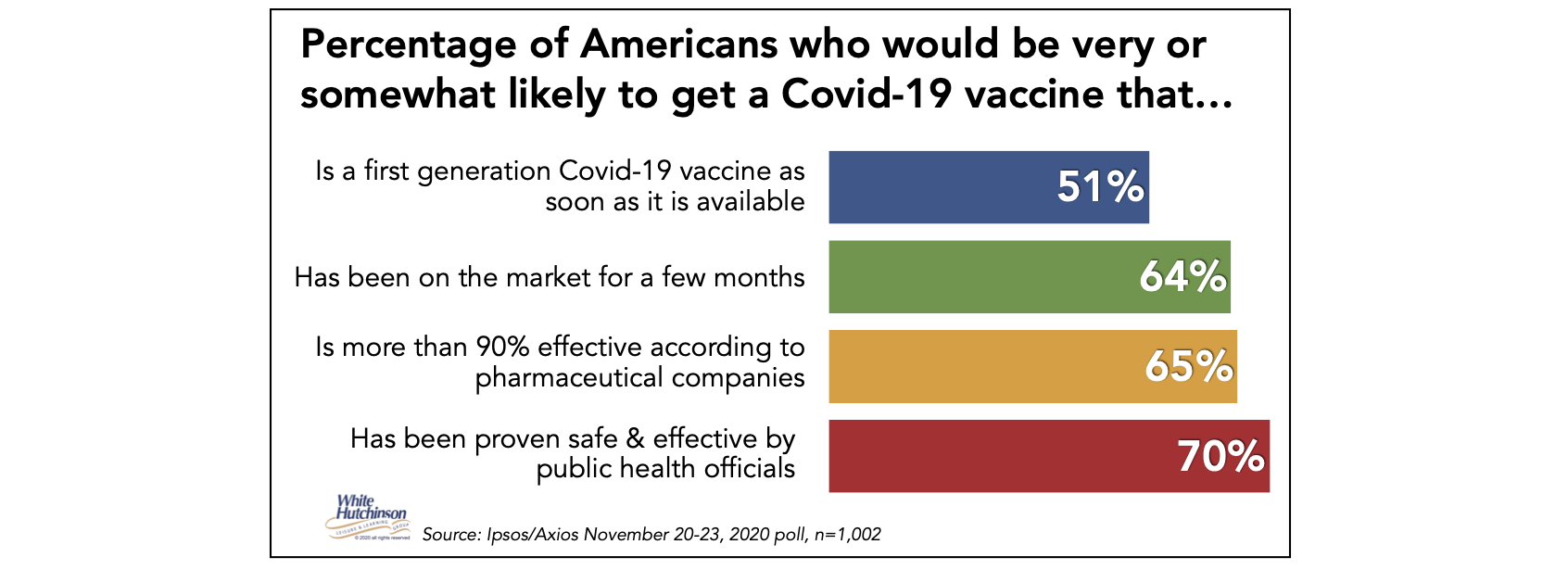
For both the Pfizer & Moderna vaccines, I used an efficacy of 94%, the lowest percentage which Pfizer found for adults age 65 and older. I’ve also included a calculation for the AstraZeneca/Oxford vaccine, which is still in Phase 3 trials and is reported to have a 62% efficacy at its regular dosing. In their November 20-23 poll, Ipsos-Axios found that 70% of adults reported that they are very or somewhat likely to get a Covid-19 vaccine that has been proven safe and effective by public health officials, up from 65% in early October. That is much higher than the 58% reported by Gallup in their October 19-November 1 poll. I’ll be optimistic and use 70%.
The highest adult vaccination rate for influenza during the past decade was achieved during the 2018-2019 flu season – 45.3%.
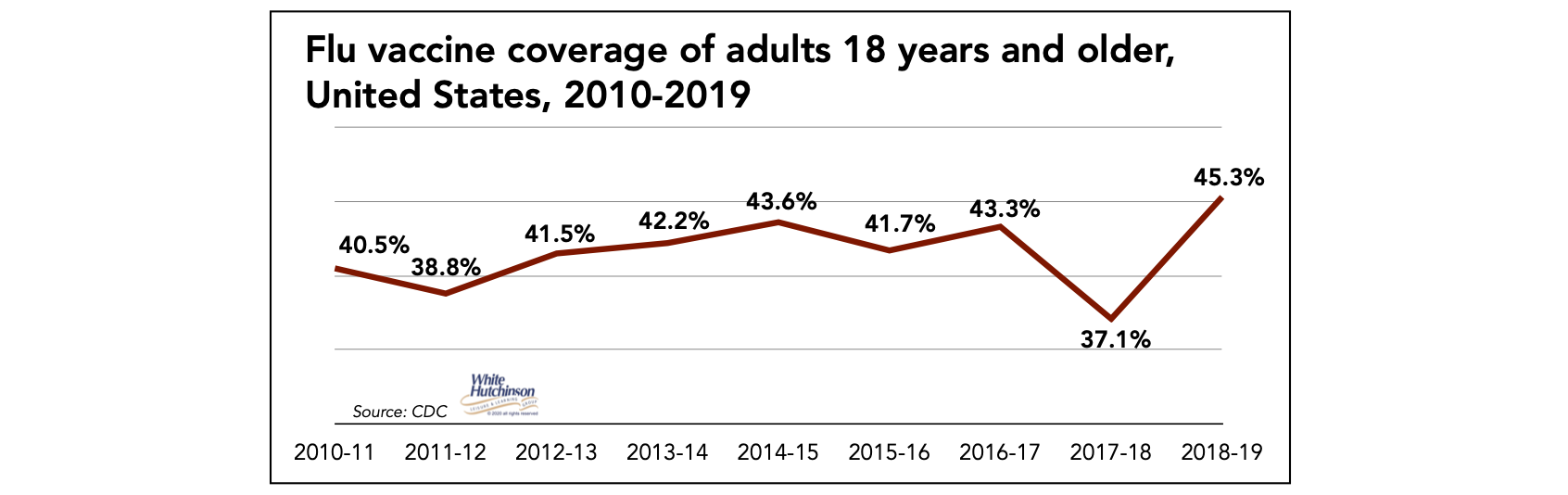
It seems reasonable that the polls are reporting a much higher vaccination intent for the coronavirus vaccine. Covid-19 is a much more serious disease than the flu; illnesses can be much more severe. The death rate is multiple times higher (10 to 40 times higher depending on the source), and many illnesses result in people known as the ‘long haulers’ with ‘long Covid,’ long-term disabilities.
I assumed that the vaccines’ effectiveness among the general population would be five percentage points lower than their efficacy. Although over 13 million Americans have been confirmed by testing to have been infected with the coronavirus, there is wide agreement that many more have been infected either with milder symptoms not requiring hospitalization or were asymptomatic. The higher estimates range from 12% to 16% of the population (the CDC just announced a new 29% estimate that seemed high compared to all the other studies I have reviewed). I assumed that more people would become infected during the vaccine’s roll-out and used a prior infection rate of 20% in the calculations. Prior infection rates vary significantly throughout the U.S. Therefore, the calculation results are an average for the U.S.
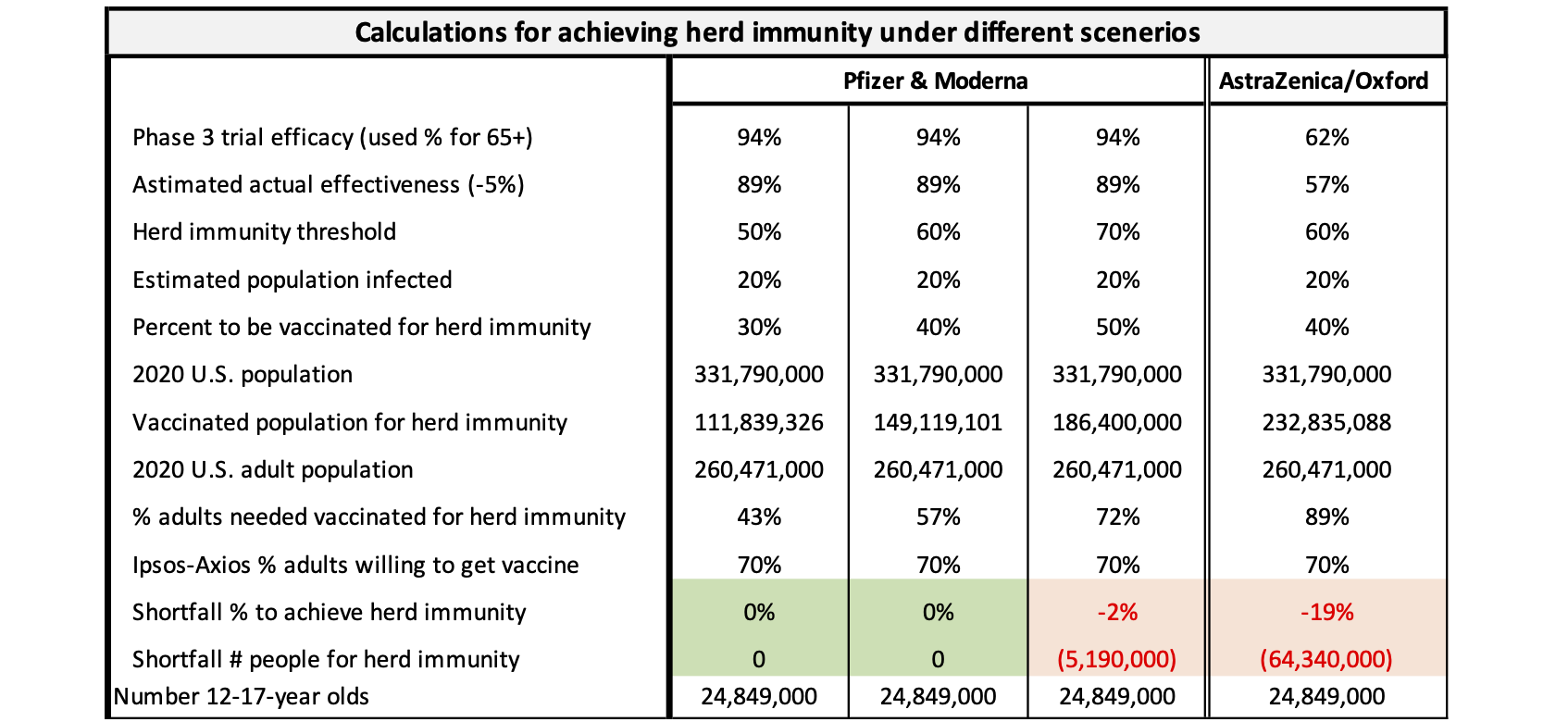
Let me walk you through the set of calculations in the third column for the Pfizer and Moderna vaccines. If the herd immunity threshold is 70% of the population and 20% are already immune due to prior infection (also assumes that immunity lasts a long time), that leaves 50% who must get immunity through vaccination. That results in 186,400,000 people needing to be vaccinated, or 72% of the adult population. If only 70% are willing to get the vaccine, that means we are over 5 million people short of reaching herd immunity. That would require some 12- to 17-year-olds also getting vaccinated, which at the earliest might not be until late 2021.
The AstraZeneca/Oxford calculation in the fourth column of the chart falls seriously short of herd immunity at a herd immunity threshold of 60%. Even vaccinating all children 12-17 won’t achieve it. An even higher threshold would make the shortfall even worse, so I saw no need for such a calculation.
You might have noticed that in the AstraZeneca calculation at a 60% herd immunity threshold, 232 million people must be vaccinated versus only 149 million for Pfizer or Moderna at 60%. Herd immunity is based on the percentage of people immune to the virus, not the percent inoculated. For Pfizer, for every 100 people who are vaccinated, 89 would be immune at 89% effectiveness, whereas for AstraZeneca, only 57 of each 100 would gain immunity at 57% effectiveness. So, far more people have to be vaccinated to equal the number needed to achieve vaccinated immunity with the AstraZeneca vaccine.
It is also essential to understand that the herd immunity thresholds assume that immune people are not infectious for any period of time. If they are, the herd immunity threshold becomes much higher, possibly unachievable, as vaccinated people can still be asymptomatic spreaders, resulting in less indirect protection for the herd.
So based on the calculations in the chart, which incorporates the assumptions of long-term immunity from both infections and vaccinations, that vaccinated people will not also be infectious, that the coronavirus will not mutate to a form the vaccine is less effective against or no longer protects against, and that we are successful with the super-cold supply chain required for distribution of the Pfizer and Moderna vaccines to the broad population, there appears to be a reasonable possibility of achieving herd immunity in the U.S. and reducing the Covid-19 infections to just an occasional level sometime late in 2021.
So, when can we stop our social distancing, take off our masks, and return to public activities? It won’t be when we start getting the vaccines. The vaccine will prevent most vaccinated people from getting ill from the coronavirus if exposed to it. But we don’t know for sure if it will protect against them infecting other people with the coronavirus. Vaccinated people may still get asymptomatic infections and thus shed the virus and possibly transmit it to others. Also, a small percentage, 11% assuming the Pfizer and Moderna vaccines are 89% effective, will not gain any immunity from the vaccine and can still get ill. People who are vaccinated will still need to social distance and wear masks the same as everyone else. That’s going to be a hard message to have people understand and follow, as they will assume a vaccine gives them immunity so they can’t get or spread the virus. It is currently difficult enough to convince some people who feel well and have no symptoms, some who will be pre-symptomatic or asymptomatic, that they need to wear masks to stop the spread.
Also, normalcy won’t return when we reach herd immunity, as the virus won’t magically disappear. It will still be infecting people. That’s not when infections stop – it’s only when they start to slow down. It won’t be until sometime after herd immunity is achieved and the Rt dramatically drops, and infections finally drop to nearly zero. That’s unlikely until sometime in the early part of 2022. And even once herd immunity is attained across the population, it’s still possible to have large outbreaks in areas where vaccination rates are low, below herd immunity thresholds.
If high vaccination rates and herd immunity is not achieved, the virus will still be around, infecting and killing people, but at much, much lower numbers. The coronavirus will become endemic at a low level, with peaks probably in winter.
If we will need to keep wearing masks and social distancing until sometime in 2022, when might we start returning to school, workplaces, and public places to socialize, party, play, be entertained, shop, exercise, and dine and drink? Fortunately, that will be sooner. There should be a gradual increase in the number of people feeling comfortable enough to return.
In the more immediate future, over the next few months, the infection rate will be a determining factor. As infection rates increase, fewer people feel comfortable visiting public places and participating in public activities, as seen from the recent surge in infections.
When infections again start to decline, more people will feel comfortable visiting public places. Other mediating factors will determine the increase to the percentage of visiting people, including the adverse economic impact the coronavirus has had on many people’s financial situations and a likely ongoing recession.
What will then have the most significant impact on returning will be the vaccines. Getting one of the highly effective vaccines will confer much higher confidence that people will be protected from the coronavirus. In the early phases of the vaccine roll-out, it will only be the health care and other essential workers that get vaccinated. That will have little if any impact on increased participation, especially in higher-risk, leisure-type public activities. Next likely will be the high-risk population vulnerable to serious illness or death from Covid due to underlying medical conditions or age. According to the CDC, approximately 60% of the population are high-risk – everyone over age 65 plus between one-third and one-half of younger age groups has one or more chronic medical conditions.
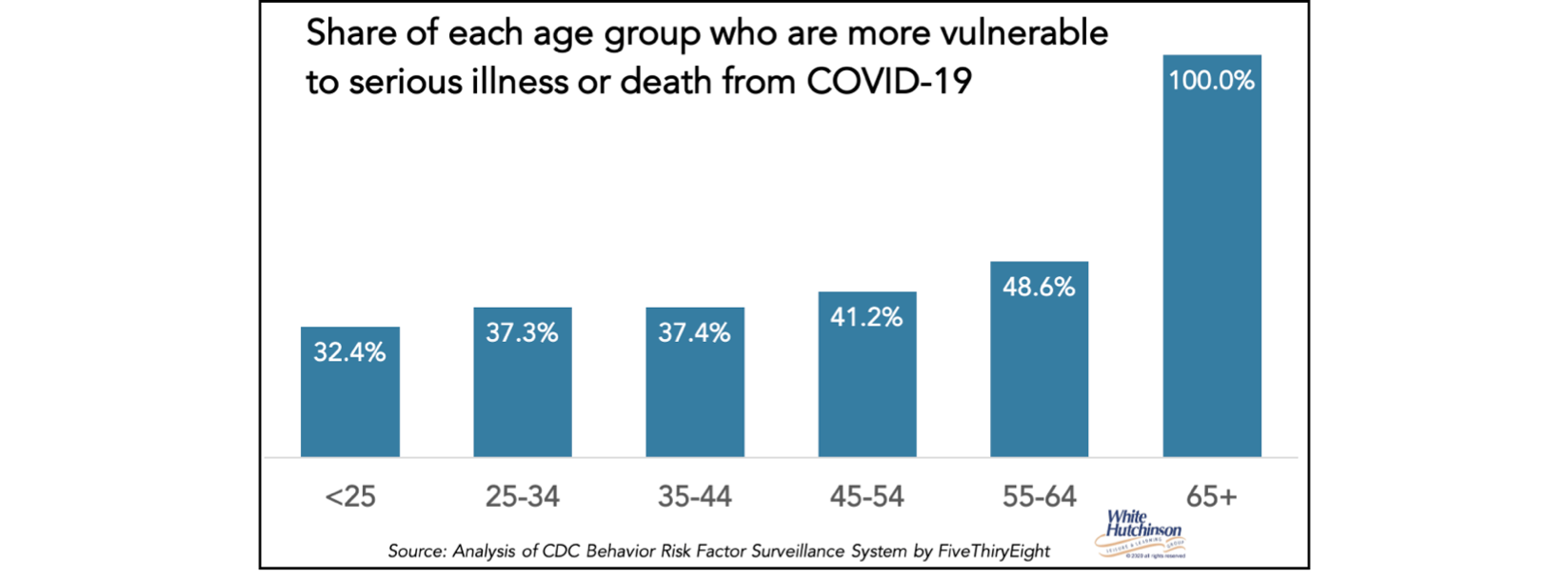
These people will continue to be risk-averse for social and public activities, as although the vaccines will reduce their risk of catching the coronavirus by about 90%, they are at high risk of serious illness or death if they do catch it. So, most will venture out more than they have, but will be very cautious. They are likely to continue to avoid higher-risk activities until herd immunity is reached. We will still need to be social distancing, wearing masks, and frequently washing or sanitizing our hands during that time.
It won’t be until the balance of the general population gets vaccinated, herd immunity is finally achieved, and a few months after that when infections will have petered out and things will get back to normal, or at least near normal. Only then can the masks come off.
But there are several caveats to that, which I will discuss in my next blog, as this one has already gotten rather long.
Follow me on Twitter and Linkedin – I try to post news and information relevant to the location-based leisure, LBE, and FEC industries a few times every weekday.
To subscribe to this blog, click here




