This is a long blog, approximately a 10-minute read. It is a must read for anyone involved with a location-based B2C business.
As we endure the impacts of the Covid-19 pandemic, including lock-downs, business restrictions, hyper-cleaning, working at home, virtual schooling, social distancing, mask wearing and obsessive hand-washing, everyone is holding out hope that a vaccine will get us to the post-pandemic world where life can return to some of the normalcy we all long for from just half a year ago. Wide press coverage of the pandemic continues to give hope that it will end by early 2021 when an effective and safe vaccine is developed. Dr Anthony Fauci, head of the National Institute of Allergy and Infectious Diseases, said he’s “cautiously optimistic” scientists will be able to create at least one safe and effective vaccine by the end of the year or early 2021.
Researchers worldwide are working around the clock to find a vaccine against SARS-CoV-2, the virus causing the Covid-19 pandemic. The New York Times’ Coronavirus Vaccine Tracker showed there are 165 vaccines under development around the world as of today, with 4 already in large scale efficacy human trials. Right now, there are vaccines under development using four different methods to trigger a person’s immune system to protect against future coronavirus infection. Additionally, there are many treatments under testing and development to help or even cure coronavirus patients while a vaccine is in development.
The purpose of a vaccine is not only to reduce a person’s risk of catching the coronavirus, but even more importantly, to get us to herd immunity. Herd immunity is achieved when a high enough percentage of a population becomes immune to a disease, such that person-to-person spread is unlikely. When most of a population is immune to an infectious disease, this provides indirect protection—or herd immunity—to those who are not immune to the disease and everyone, not just those immune, are protected.
To achieve herd immunity, a certain percentage of the population has to become immune, either through prior infection or vaccination. Different vaccines may offer different levels of protection, referred to as the vaccine’s efficacy or effectiveness. If 100 vaccinated people are exposed to a virus with a vaccine that is 70% effective, that means on average 70 of them will not get infected, but 30 will if exposed to the virus.
The difference between efficacy and effectiveness is that the former applies when vaccination is given in a clinical trial, and the latter is under “real-world” conditions. Typically, a vaccine’s effectiveness tends to be lower than its tested efficacy.
The measles vaccine has an efficacy of 95%-98% required due to its high rate of contagion. Flu vaccines are in the range of 20% to 60%. The 2017-2018 flu vaccine was 38% effective.
Dr. Fauci said he would “settle” for a coronavirus vaccine that’s 70% to 75% effective taken by two-thirds of American, as that would bring the United States to “herd immunity level.”
The lower the percentage of people that get inoculated, the higher the vaccine efficacy has to be to achieve herd immunity. A study published July 15 in the American Journal of Preventive Medicine found that a coronavirus vaccine’s effectiveness may have to be higher than 70%, or even 80%, when vaccinations are only at 60% for Americans before we can have herd immunity and can safely stop relying on social distancing measures.
Some epidemiologists and mathematicians are using a heterogeneous model to predict required effectiveness. A heterogeneous mode predicts highly susceptible people are more likely to get infected first, so as a result, the average susceptibility gets lower and lower over time (rather than in a homogenous model that assumes all people are equality susceptible to the virus). Heterogeneous models are coming up with between 20% and 60% required vaccine effectiveness.
The US Food and Drug Administration (FDA) sets licensing standards of vaccines. The FDA says it expects vaccines to demonstrate at least 50% efficacy to be licensed and widely deployed against Covid-19.
One clear caveat all the models make is that after infection or vaccination, people obtain long-term immunity, which may not be the case as discussed later.
According to the CDC, during the 2019- 2020 flu season, 62.6% of children 6 months through 17 years and less than half of adults (45.3%) got the flu vaccine. They found that general vaccine hesitancy, distrust of vaccine safety, and vaccine novelty are among the most important deterrents to vaccination.
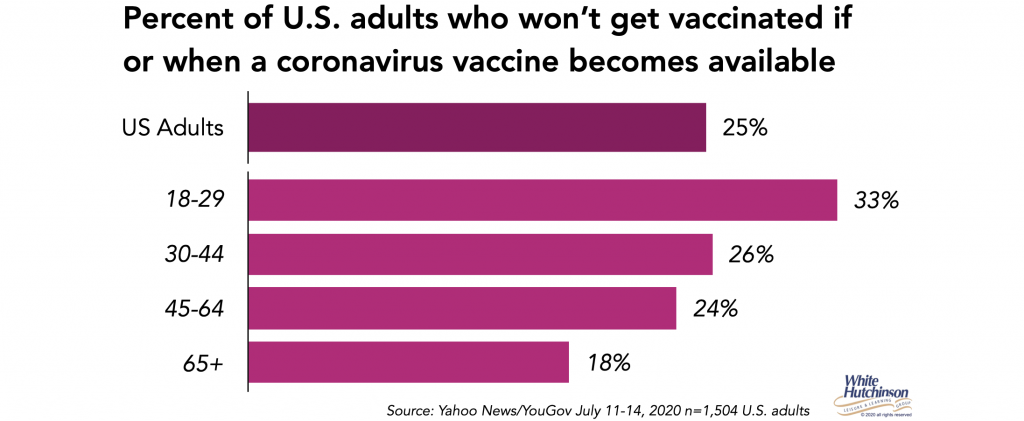
As optimistic as Dr. Fauci is about the quick development of a vaccine, he says it is “unlikely” that the US will achieve sufficient levels of immunity to quell the outbreak as it appears that too many people will refuse to get the shot when it’s available because of a “general anti-science, anti-authority, anti-vaccine feeling.” Yesterday, Dr. Fauci said “I don’t think really see us eradicating it.” He did say that it’s possible to bring it down to “low levels.” Peter Marks, director of the Center for Biologics Evaluation and Research at the FDA, said that one of the things that “scares me more than anything else is that a third or half of Americans are hesitant about taking a vaccine [for Covid-19].”
A YouGov poll this month found that one-quarter of adults will not get a coronavirus vaccine. Only 46% answered they would get the vaccine. The remaining 28% answered they were “not sure,” indicating some of them may eventually fall into the “not” category.
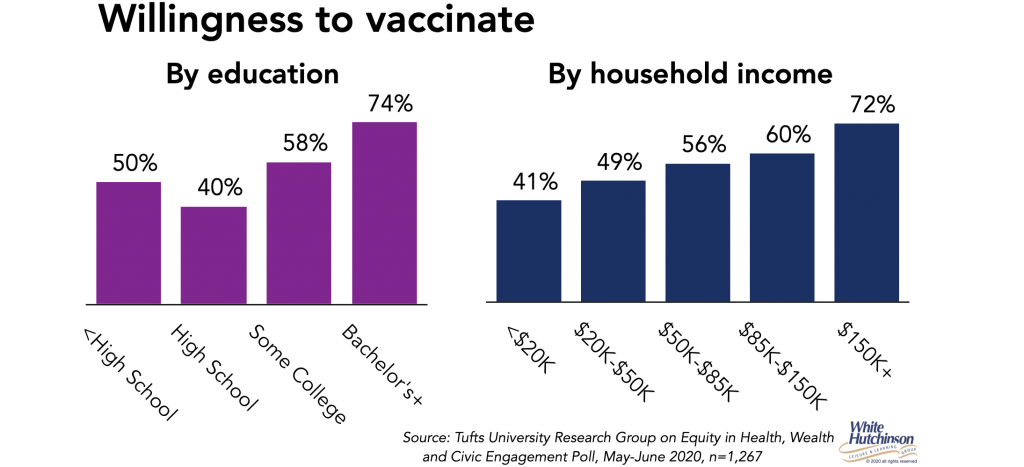
A Tufts University Research Group’s May-June poll found that 18% of adults said they won’t get vaccinated and 24% were undecided. Here’s the breakdown of the willingness to get vaccinated from their poll. The lower socioeconomic, who are the majority of essential workers and at heightened risk of catching the virus, have the lowest willingness to get vaccinated.
Analysis by the independent organization Media Matters found that the three most prominent anti-vaxxer groups in the United States are already laying the groundwork for “widespread coronavirus vaccine rejection.” Facebook pages for the groups are “rife with vaccine conspiracy theories and other coronavirus misinformation.”
All this doesn’t mean that a vaccine with a lower efficacy or a low vaccination rate would not be useful. But it would mean that social distancing, mask-wearing, restricted group size and other measures likely would have to continue until a vaccine that is actually “good enough” arrives with high rates of inoculation.
Developing a Covid-19 vaccine in record time, producing enough and inoculating enough people to end the pandemic will be the biggest medical feat in history.
The critical timeline for a Covid-19 vaccine is just not to get to its licensing, but how long it will take for a sufficient percentage of the population to be vaccinated. It’s not a small feat to manufacture a vaccine for billions of people and then rapidly get it to all of those people throughout the world. When a vaccine is ready, there will be major supply chain challenges for widely distributing the shots worldwide.
A number of vaccine developers are already manufacturing them at risk, so if they prove safe and efficacious, there will already be a supply to start distribution. Dr. Fauci believes final trial results for a number of vaccine candidates could come in the late fall or early winter. Moderna, developing one of the more promising vaccines, believes they will produce enough vaccines in a year to vaccinate everybody in the U.S. (their vaccine requires two doses 28 days apart). If all that falls in line, it still wouldn’t be until no sooner than late 2021that everyone who is willing to get vaccinated can be.
Companies and governments are racing to scale-up machinery to address a critical shortage in the automated capacity of putting the vaccine into vials or syringes, sealing them and packaging them up for shipping. Adding to the challenge is that glass vials are in short supply. A medical-glass shortage was looming before the coronavirus crisis hit. Rick Bright, former director of the federal Biomedical Advanced Research and Development Authority (BARDA), believes securing enough to vaccinate 300 million Americans could take up to two years.
Several vaccine developers are experimenting with new ways to mitigate the extreme cold storage requirements of some vaccines, which at present need to be kept at minus 112 degrees Fahrenheit, presenting another challenge. Most pharmacies, clinics and doctor’s offices don’t have that cold storage ability. Companies developing mRNA vaccines are working to make candidates stable at higher temperatures. Moderna hopes to add a small period of time in which their vaccine can be stored at normal fridge temperatures at vaccination sites. Another company is working on producing vials that won’t shatter at super-cold temperatures. (learn more Vaccine makers face biggest medical manufacturing challenge in history). From managing extremely cold storage conditions, and even inventing and manufacturing new kinds of vials and syringes, the path forward is strewn with formidable hurdles.
“In order to stop the pandemic, we need to make the vaccine available to almost every person on the planet,” Bill Gates, Co-chairman and co-founder of the Bill & Melinda Gates Foundation, says. “We’ve never delivered something to every corner of the world before.” The consideration is that if other countries, especially low-income ones, don’t get fully vaccinated, coronavirus will keep getting reintroduced into the high-income ones.
There is one more unknown for whether even a highly effective vaccine given to a large enough segment of population will get us to herd immunity. There is a serious question about how long immunity lasts and how soon people can be reinfected with Covid-19. Both recovery from coronavirus and a vaccine produce antibodies to fight off infection. The shelf life of those antibodies may not last long enough to protect people with long-term immunity while the population is being vaccinated. For example, if it took one year to vaccinate the entire population, the people vaccinated at the beginning could lose their immunity mid-way through the roll-out, thus defeating the Holy Grail of achieving herd immunity and stamping out Covid-19.
Other coronaviruses, such as the flu, demonstrated people were just as likely to be reinfected a year later as people who were never infected. Preliminary studies show that not all patients develop antibodies after infection and COVID-19 antibodies decline in patients after a few months. There are a number of reports of Covid-19 patients getting reinfected. This raises the possibility that in addition to initial immunization, periodic booster shots will be required to maintain continued immunity.
The Covid-19 immunity that’s been tested is based on antibodies. Some hold out hope that a vaccine that also produces a lot of disease-fighting T-cells, which work differently than antibodies and last longer, will afford longer protection.
There is one more unknown about the coronavirus. Will it mutate so that the current vaccines under development won’t be effective when they are ready or soon after they are deployed?
More than 6 months into the pandemic, the virus’ potential to evolve in a nastier direction—or, if we’re lucky, become more benign—is unclear. In part that’s because it changes more slowly than most other viruses. On average, the coronavirus’ genome accumulates about two changes per month. Most of the changes don’t affect how the virus behaves, but a few may change the disease’s transmissibility or severity.
At some point early in the pandemic, one of the 30,000 letters in the genome of SARS-CoV-2 changed from an A to a G. Today, that mutation has spread around the world. It has become the center of a burning scientific question: Has the mutation become so common because it helps the virus spread faster? Or is it just coincidence?
The big question is whether we’ll be able to vaccinate for Covid-19 once and then you never have to get it again (setting aside the issue of how long immunity lasts), or will it be something that will require a new vaccine you have to get every year or so to keep your immunity up to date, just like needing an annual flu vaccine.
Just how deadly is the coronavirus? Epidemiologist Gideon M-K examined the infection-fatality ratescalculated as deaths as the proportion of infected people estimated from serological testing for both Covid-19 and influenza. He found that “it looks like COVID-19 has a fatality rate roughly 50–100 times higher than influenza. In other words, between 1 and 10 in 100,000 people who get the flu will die, but between 500 and 1,000 in 100,000 people who get Covid-19 will pass away.” Other researchers have come to a similar conclusion.
A large portion of the population is vulnerable to severe Covid-19 illness or death. In addition to everyone over age 65, nearly 40% of all Americans under 65 have a condition that makes catching coronavirus very dangerous to them.
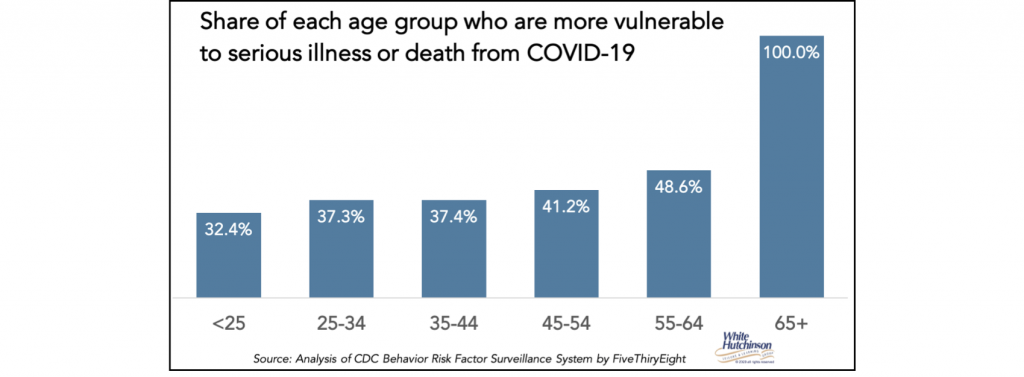
The “CDC now warns that among adults, risk increases as you age, and it’s not just those over the age of 65 who are at increased risk of severe illness.”
But even after surviving the initial infection, Covid-19 can bring severe illness that can take a long time to recover from. Some people have symptoms that persist for months, known as “Covid-19 long-haulers.” Dr. Fauci reports potentially debilitating Covid-19 post-viral syndrome that includes “brain fog, fatigue and difficulty in concentrating.” The coronavirus isn’t like the regular flu where everyone who gets it recovers quickly.
People in the U.S. are worried about catching the coronavirus. These three polls taken within the last month found that between a little over one-half to three-quarters of adults are worried about personally getting sick from the virus.
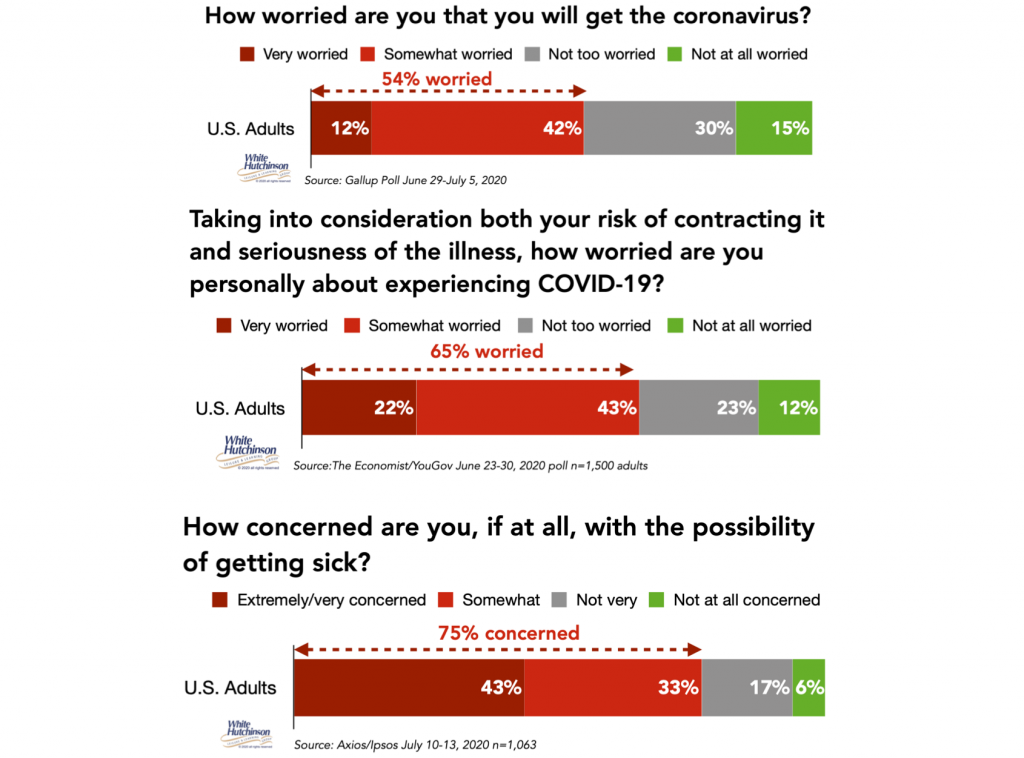
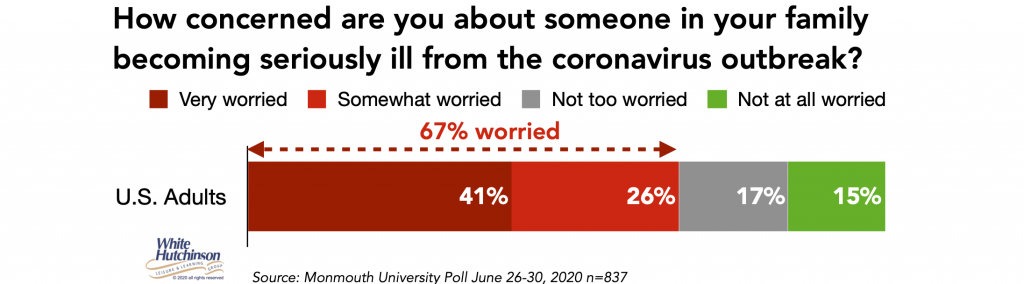
Two-thirds are worried about someone in their family becoming seriously ill from the virus.
A just released July 17-19 Harris poll found that more than half of adults (54%) fear they could die as a result of contracting the coronavirus. Nearly three-quarters (72%) are very/somewhat concerned that leaving their home to go to non-essential businesses (e.g. bars, hairdressers, cinemas, etc.) would risk exposing them, their loved ones, or others to the coronavirus.
In all four polls, less than one-sixth report they are not at all worried (maybe they are all the young adults who continue to party, not socially distance and not wear masks).
A July 10-13 Ipsos poll found that 70% of adults think that there is a large or moderate infective risk of currently returning to their normal pre-Covid life.
People increasingly know people who have tested positive for Covid-19 or died from it. One sixth of adults personally know someone who has died from the virus. 4 in 10 know someone who tested positive.
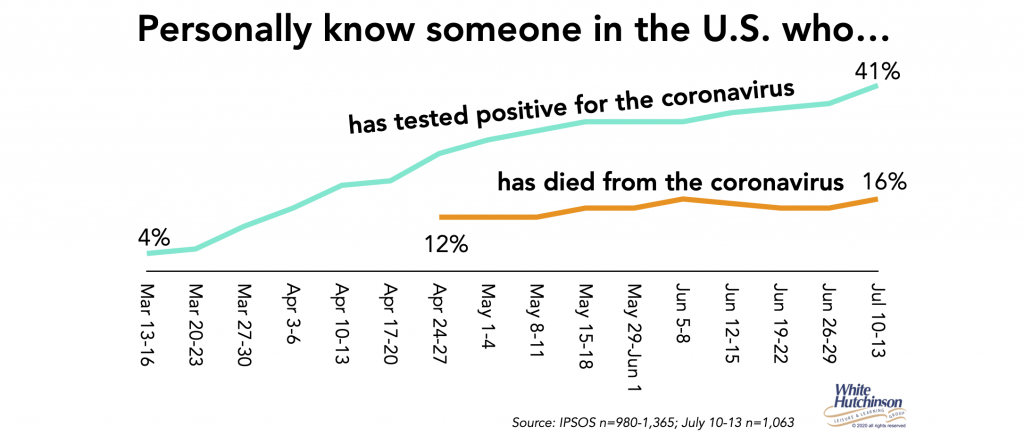
As people increasingly have personal knowledge of people experiencing the virus and its possible severity, the percentage with personal concerns that they or a member of their family will catch the coronavirus will probably increase, negatively impacting their willingness to venture out into public places they consider risky.
Currently 1 in 5 people say they won’t go back to normal day-to-day activities until after a vaccine is developed. Another 29% say they will wait until there are no new cases in their state, which for all practical matters means a vaccine to get to herd immunity.
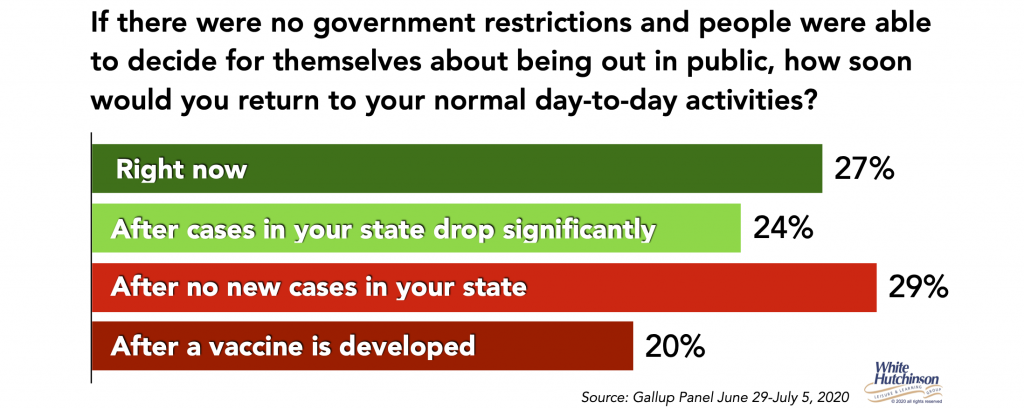
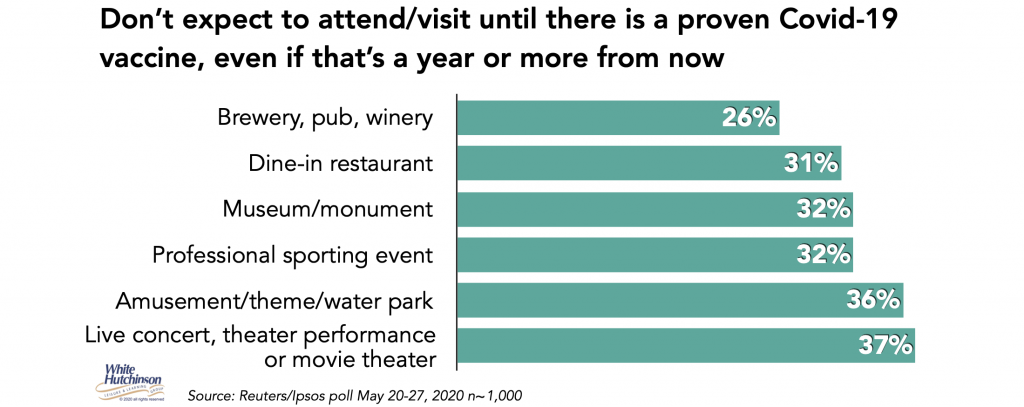
A Reuters/Ipsos poll found a third or more of adults said they won’t attend entertainment and cultural venues until there as a vaccine, even if that’s in a year or more.
All the people that say they will not do many things until there is a vaccine are really saying they won’t until they get a vaccine that protects them or there is herd immunity. Unless a vaccine is near 100% effective, they probably won’t consider it protects them even if they get vaccinated. If a vaccine was 70% effective, for the average person, that would only reduce the odds of dying from Covid-19 to 15 to 30 times more than the flu, still not very good odds. The older people are, the worse the odds become. Plus, they would still have a high probability of catching it and infecting a family member.
All indications point to the post-pandemic world being much further in the future than people hoped. With all the uncertainty about developing a vaccine with a high enough effectiveness, whether it will give long-term immunity, whether it will mutate, how long it will take to manufacture, distribute and vaccinate enough people to get to herd immunity, the timing is uncertain. In the U.S., with so many people refusing to take a Covid-19 vaccine, we may not get to herd immunity and will have to live with the virus for a very long time. Even if all the stars perfectly line up, it looks like the earliest we could get to herd immunity and close the book on Covid-19 is late 2021.
In the meanwhile, life will continue to require social distancing, wearing masks, regular handwashing and avoiding crowds, especially indoors, to keep the virus under control. And a large percentage of people, especially those most at risk or with family members at risk, will definitely avoid many public places, including location-based entertainment, cultural venues and dining indoors at restaurants.
Location-based B2C businesses, including entertainment/cultural venues and restaurants, need to innovate and adapt their business models to survive not just until we get a vaccine, but until there is herd immunity, which is at least 1.5 years, and probably even longer away. And there is the strong possibility we may never get to herd immunity and eradicate Covid-19. We may have to learn how to live with the coronavirus at some level forever.
Follow me on Twitter and Linkedin – I try to post news and information that is relevant to the location-based leisure, LBE and FEC industries a few times each weekday.




