Vol. I, No. 1, March 2023
The E. coli 0157 menace: Designing and operating safe animal petting areas
This is a long article, but well worth a read if you want to have a safe animal petting area.
Animals are an endless source of wonder for children. There are few, if any, attractions that have a greater appeal to young children than animals. Research shows that young children feel a natural kinship with and are implicitly drawn to animals, especially baby animals. Children interact instinctively and naturally with animals, talk to them, and invest in them emotionally. Studies show that as many as 80% of the dreams of children younger than 6 are about animals. Additional evidence of animals' importance to children is that animals constitute more than 90% of the characters in children's preschool books. That is why animals and animal petting areas, sometimes called petting zoos, are so popular at agritourism farms as they are a magnet for young children who bring their parents with them.

Farm animals that children can interact with - feed, pet, and groom - can be the foundation, a main attraction for agritourism facilities that target families with children. The truth is adults also enjoy watching and interacting with animals. Unfortunately, animals can also pose serious risks to children in the form of both injury and illness if the animal area is not correctly designed, managed, and maintained.
Preventing physical injury from animals that interact with children can be addressed by selecting appropriate and more docile breeds, using younger animals, proper design and fencing, and providing appropriate supervision.
However, what poses the most significant risk to agritourism visitors and to the very economic survival of agritourism businesses is not the animals themselves. It's the microscopic organisms that animals can harbor, especially Escherichia coli 0157:H7, better known as E. coli 0157:H7 or just E. coli 0157. Outbreaks of E. coli 0157 can result in dire consequences for the farm's owner, as parents can boycott the facility, liability insurance can become very expensive or unobtainable, and the agritourism farm could go out of business. Furthermore, every outbreak increases parents' fears and reluctance to visit agritourism facilities with animals, hurting the entire industry. Even one outbreak hurts the industry as a whole.
Most often, it's infants and young children who become ill due to their underdeveloped immune systems and poorer hygienic practices compared with adults, such as more frequent hand-to-mouth behaviors. However, illnesses are preventable if the petting areas are correctly designed and managed.
E. coli was first identified in 1885. E. coli is found in the intestines of both humans and animals. The organisms colonize the human intestinal tract shortly after birth and usually do not cause illness. Instead, they serve the beneficial purpose of suppressing the growth of harmful bacteria and aiding in the synthesis of vitamins.
E. coli had been quietly doing the job of protecting people from harmful intestinal bacteria for eons. But sometime in the early 1970s, scientists believe the mutant strain E. coli 0157:H7 was created when a virus infected benign E. coli and gave it a string of DNA from Shigella, a bacterium that causes severe, bloody diarrhea. The first case of E. coli 0157 illness was reported in 1975.

E. coli 0157:H7
E. coli 0157 came into the public limelight in 1993 when more than 700 people became ill from eating contaminated hamburgers at 90 Jack-in-the-Box restaurants in four western states. Some 200 people had to be hospitalized, and four children died. Since then, numerous outbreaks have occurred from undercooked contaminated hamburgers. Then in 1996, 70 people fell ill from unpasteurized apple juice contaminated by apples dropped on the ground that came into contact with manure or by apples sprayed with contaminated groundwater. Over half the cases were children under age 6, one of whom died.
In 1990, the first reported outbreak of E. coli 0157 transmitted by contaminated drinking water occurred in southern Missouri, with 243 cases and four deaths. In addition to hamburgers, apple juice, and drinking water, illnesses from E. coli 0157 have been attributed to contaminated pool water, unpasteurized milk, and various vegetables and fruits that were either irrigated or washed with contaminated water.
E. coli 0157 causes human illness through the toxins that it produces that destroy the intestinal wall. The illnesses range from mild cases of acute diarrhea to death. Most infections are mild and don't require medical care. Acute illness from E. coli 0157 includes abdominal cramps, vomiting, diarrhea (often bloody), and sometimes fever. However, some cases can result in hemorrhagic colitis (bloody colon inflammation). In addition, a small percentage of cases (approximately 8% of all E. coli 0157 infections) develop hemolytic uremic syndrome (HUS), a life-threatening disease characterized by red blood cell destruction, kidney failure, and neurological complications, such as seizures and strokes. People who develop chronic kidney failure may require lifelong dialysis or a kidney transplant. Children under five years old who have not yet fully developed their immunities are especially susceptible to both E. coli 0157 and the development of HUS, which is the leading cause of kidney failure in children in the U.S. Of children affected with HUS, 3% to 5% will die. As many as 30% will have lifelong medical problems.
It takes only as few as ten germs of E. coli 0157 to cause illness, whereas it takes about a billion salmonella bacteria to make you sick. Symptoms of E. coli 0157 exposure develop within 5 to 9 days of exposure, and people infected usually recover in 5 to 10 days. The Centers for Disease Control (CDC) reports that about 200 people a day get ill from E. coli 0157, and a little over an average of one person a week dies from the illness. Only about one-tenth of one percent of all E. coli 0157 infections occur in animal petting areas. However, since the vast majority of illnesses occur in very young children, outbreaks receive wide press coverage and, as a result, heighten parents' fears of visiting animal petting areas.
Although the largest number of E. coli 0157 illnesses are attributed to food contamination, studies by the CDC show the highest risk (probability of being infected) is from exposure to farm animals, especially cattle.

Cattle pose the highest risk of infecting agritourism visitors with E. coli 0157
Other ruminants like sheep and deer can also carry the organism. The growing populations of deer are believed to be responsible for spreading E. coli 0157 to farm animals in many areas. Even dogs, chickens, goats, and pigs have been found to harbor E. coli 0157. It is believed those animals become contaminated by exposure to cattle manure or deer feces. E. coli 0157 is excreted in the manure or feces and can survive for long periods of time on the ground or the hides of animals. Anything that comes into contact with cattle manure can be contaminated, including ponds, lakes, streams, and groundwater by field runoff.
A single cow produces about 66 pounds of manure daily. Each gram of manure can contain ten million (10,000,000) fecal E. coli organisms. Therefore, a single cow can produce about three hundred billion (300,000,000,000) fecal E. coli per day, which could include E. coli O157.
Research shows that E. coli 0157 can live for months in animal bedding and soil. E. coli 0157 infections have been traced to manure dust in areas where cattle had been removed 10 days earlier. Contamination from airborne dust was implicated in an Oregon county fair outbreak that sickened 60 people, mostly children, none of whom had touched animals.
Among cattle, up to 50% can be contaminated, with the highest rates occurring in the summer. Studies by the U.S. Department of Agriculture have found animals testing positive for E. coli 0157 in every herd that has been tested. Other studies have found E. coli 0157 on the hides of 11% of cattle entering meat-processing plants. A 2003 study on the prevalence of E. coli O157 in livestock at 29 counties and three large state agricultural fairs in the United States found the organisms in 13.8% of beef cattle, 5.9% of dairy cattle, 3.6% of pigs, 5.2% of sheep, and 2.8% of goats. Complicating matters is that infected animals show no symptoms and do not become ill. Further, farm residents have a much lower risk of infection than non-farm residents, probably because they acquire immunity to the illness due to their childhood and frequent exposure to the organisms. Therefore, there is no way to know that animals are infected, especially on farms where farm residents and workers rarely become infected.
The first reported cases of E. coli 0157 illnesses from agritourism animal petting areas occurred in 2000. At the Merrymead Farm outside Philadelphia, at least 61 people became infected, and almost all children were under 11. One 3-year-old suffered kidney failure, and a 2-year-old and a 4-year-old developed hemolytic uremic syndrome that can require dialysis. The CDC linked the E. coli 0157outbreak to cows and calves at the farm's petting zoo. Also, in that same year, an outbreak at a farm in Snohomish Country, Washington sickened three children. The CDC did an exhaustive scientific study of both outbreaks and traced the infections to children petting animals or just touching the railings of the animal pens.
The most recent child death from E. coli 0157 related to an animal petting area occurred in Rutherford County TN in 2022, when a 2-year-old died. The Tennessee Department of Health said the child's older brother attended summer camp at Lucky Ladd Farms where he picked up E. coli. 0157. The bacteria were then transmitted to the 2-year-old, who developed hemolytic uremic syndrome and died. The TDH also found that two other children who attended the summer camp got ill. The source of E. coli 0157 was traced to two baby goats that were in contact with the confirmed cases.
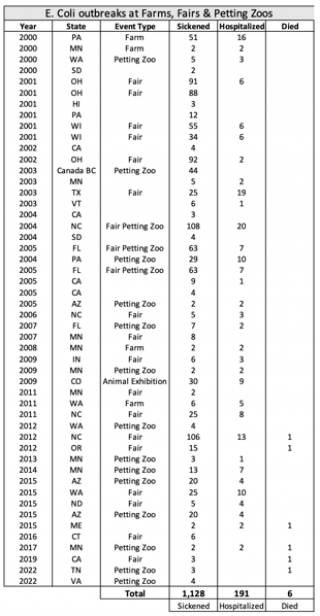
Since from 2000 through 2023, there have been at least 50 incidences of visitors getting sick from E. coli 0157 at petting zoos and animal petting areas in North America, with 1,128 children and adults getting ill with over 191 being hospitalized and at least six deaths.
Many studies have examined the behaviors associated with illness from E. coli 0157 at petting zoos. One study by the CDC and Florida Department of Health of two petting zoos that sickened at least 34 people found the behaviors most strongly associated with illness are feeding a cow or goat, touching a goat, and stepping on manure or having manure on your shoes. Indirect contact that also led to illness included drying hands on one's clothes after washing them. The research found that people who washed their hands after visiting the petting zoo, including lathering with soap, and then rewashing them before eating escaped illness.
In another study, a team led by Amy E. Belflower, an epidemiologist at the South Carolina Department of Health and Environmental Control, watched 227 people in a petting zoo to see how many washed their hands or engaged in risky behaviors. The petting zoos followed recommended guidelines, Belflower said. "They had the animals in pens, had signs about not bringing food and drink in, and lots of signs about washing your hands, and had good handwashing stations. But even with all those precautions, we still saw people engaging in risky behavior. The top three were bringing food into the area, bringing a stroller into the area, and picking stuff like pet food off the ground. We also saw that 28% of the people who exited the petting area did not wash their hands."
A study by researchers from the Tennessee Department of Health and the U.S. Department of Agriculture also looked at how people behave in petting zoos. Among 991 visitors to six petting zoos in middle Tennessee, they found that:
- 49% of visitors touched their faces while in the petting zoo,
- 87% came into contact with environmental surfaces such as handrails or benches,
- 74% touched animals,
- 22% ate or drank while in the area, and
- 62% did not wash their hands after leaving the petting zoo.
A 2013 observation study identified some of the most common risk behaviors visitors performed in 13 petting zoos in the United States. These included touching hands to face in animal areas, animals licking hands, and eating or drinking within animal-contact areas. Other risk factors linked to E. coli 0157 infections include children touching their mouths, putting objects in their mouths, biting their nails, having contact with manure, sucking thumbs, eating, or having soiled hands and shoes during or after being in animal-contact areas.
The primary mode of transmission of pathogenic E. coli is the fecal-oral route. Since animal fur, hair, skin, and saliva can become contaminated with fecal E. coli 0157, transmission can occur when persons pet, touch, or are licked by animals. Most children's illnesses are caused by hand-to-mouth transfer of E. coli 0157 after touching or being licked by animals. Young children will pet a sheep, goat, or calf, touch a contaminated surface, sit or fall on contaminated ground, and then put their fingers into their mouths or touch the food they're going to eat. Research by the CDC and state agriculture departments of E. coli 0157 outbreaks at animal petting areas attribute illness almost entirely to hand-to-mouth or hand-to-food (or pacifier) to mouth transfer.
The single most important preventative measure guests can take is handwashing. Not having calves, cows, or other ruminant animals and young poultry in petting areas also significantly reduces risk.
In addition to E. coli 0157, salmonella, which causes diarrhea, fever, and abdominal cramps; cryptosporidium, a parasite that causes diarrhea; and campylobacter that causes diarrhea, fever, and stomach cramps are also commonly reported illnesses passed from animals to humans. However, due to the low infective dose of E. coli 0157 and the severity of illness that can develop, particularly in young children, E. coli 0157 is the pathogen of utmost concern at animal petting areas.
Animal petting area operators can significantly reduce the risk of E. coli 0157 or other animal-transmitted pathogenic illnesses through the physical design and management of their facilities:
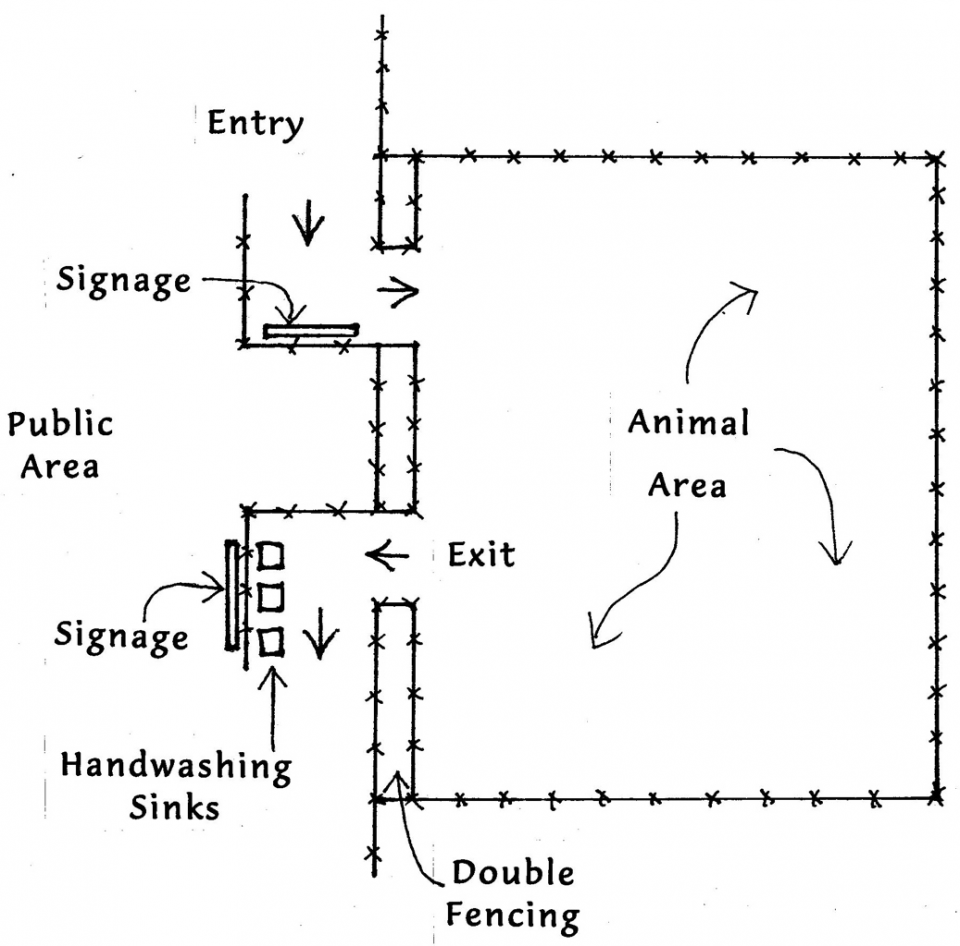
- Animal contact areas should be designed to be separated by some distance, fenced, and gated from play and eating areas. This includes double-fencing in areas where guests could touch animals from outside the designated animal area.
-
 Materials used to construct animal areas and pens visitors can come
in contact with should be non-porous, such as metal rather than wood,
allowing more effective sanitization. Railings and fences visitors can
contact should be cleaned and disinfected regularly.
Materials used to construct animal areas and pens visitors can come
in contact with should be non-porous, such as metal rather than wood,
allowing more effective sanitization. Railings and fences visitors can
contact should be cleaned and disinfected regularly. - There should be entry and exit transition areas. The entry area should include signage about the risk of contact with animals and educational information on the heightened risk for children five and younger, people with a high risk of infection or reduced immunity, and persons who are cognitively impaired or pregnant. Information should tell parents how to minimize risk to their children, including not allowing children to put their fingers in their mouths. Food, beverages, smoking, carry toys, strollers (so the wheels won't carry E. coli picked up from the ground to outside the animal area and possibly home), pacifiers, spill-proof cups ("sippy cups"), or baby bottles should not be permitted in the animal areas. The sign should be positioned to face people as they enter the animal area so it can't be missed.
-
 Have a clearly marked designated area near the entrance for visitors
to leave strollers and related items (e.g., wagons, diaper bags, toys,
pacifiers, and baby bottles).
Have a clearly marked designated area near the entrance for visitors
to leave strollers and related items (e.g., wagons, diaper bags, toys,
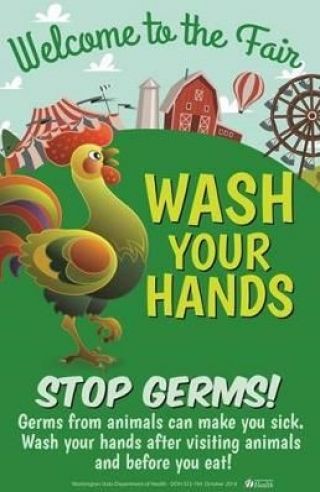
pacifiers, and baby bottles). - The exit area should have adequate handwashing sinks (including ones low enough at 22" for easy use by children) with running water, liquid soap dispensers, and disposable paper towel dispensers within reach of each sink. Clear signage should instruct all guests to wash their hands and for parents to assist their children with handwashing. The handwashing stations and signage should be positioned straight out of the exit gate so exiting people face it and it can't be missed (see diagram). Handwashing signs should be readable at a distance, use bulleted text, and graphics illustrating handwashing, and be multilingual if possible. Hand sanitizers are not considered an acceptable alternative to handwashing at animal areas.
-
 Ensure enough handwashing sinks are available for the expected
number of visitors during anticipated peak attendance. If lines at
handwashing stations are long, visitors may not wash their hands or may
wash quickly to keep the line moving.
Ensure enough handwashing sinks are available for the expected
number of visitors during anticipated peak attendance. If lines at
handwashing stations are long, visitors may not wash their hands or may
wash quickly to keep the line moving. - Schedule staff to monitor the handwashing station to encourage all visitors to wash their hands when leaving and ensure that soap and paper towels are always available.
- Limit the maximum number of visitors allowed in the petting area at crowded times. When the petting area is crowded, visitors are less likely to see handwashing signs and handwashing stations or are less likely to wait in line to wash their hands.
- Animals should be kept clean, and hay, urine, soiled bedding, and uneaten food should be removed regularly. Manure should be removed on a timely basis. If it becomes dry, subsequent air movement can result in the airborne spread of manure dust, which could spread infectious E. coli 0157 onto surfaces and into public areas.
- In the animal areas, animal feed and water, shovels, pitchforks, and other tools to remove animal bedding should not be accessible to the public.
- If feeding animals is permitted, only food sold at the venue for that purpose should be allowed. Animal food should not be sold in ice cream cones that children might eat.
- Animals that are not safe for children to interact with should be double-fenced. A slanted feed tube can be put in the fence to allow people to drop feed into it.
- The Americans with Disabilities Act (ADA) requires animal petting areas to be accessible by people with disabilities. This means there must be accessible paths (walkways that people in wheelchairs can traverse). So unlike strollers that can be restricted from animal areas, wheelchairs, and other mobility assistance devices cannot. Have a place where wheelchairs and mobility devices can be sanitized after leaving the animal area. Procedures should be established for staff to assist people with sanitizing any parts of the devices that come in contact with animals or the ground upon exiting the animal area.
- Animal areas should be supervised by staff trained on how to minimize risk and intervene with children and parents whose children are not following safe practices.
- Animals should be monitored daily for signs of illness and ensure that animals receive appropriate veterinary care. Ill animals, animals known to be infected with a zoonotic pathogen, and animals from herds with a recent history of diarrhea or respiratory disease should not be exhibited. To decrease the shedding of pathogens, animals should be housed in a manner to minimize stress and overcrowding.
- Food and beverage areas should be separated, distant, and uphill (to prevent contamination by groundwater runoff) from animal areas and have additional clearly visible outdoor handwashing facilities available.
- Pony ride areas should also follow the above standards.
- Farm ponds that the public can access should not be located where animals can access them or where water can become contaminated by runoff from fields or other areas that contain animals or by animals visiting the pond.

E. coli 0157 can be spread by pasture water runoff into ponds & streams.
- Agritourism farms that offer animal contact should:
- Post information on their websites about the risks from animal contact and include educational material for parents on how to minimize risks when visiting
- Post signs with similar information at the entry to the facility
- Offer a handout parent guide upon entry to their facility on how to enjoy the facility and properly supervise their children's interaction with animals. This handout can include other information for parents about how their family can best enjoy their stay at the farm, a map of the facility, perhaps a farm history, and additional helpful information.
- For school groups, supply the schools with information about the risk of infection when interacting with animals and the importance of handwashing to go home with permission slips. Have staff review safety measures with students and chaperons before they exit the bus or before they enter the animal petting area.
Farm animals are a powerful magnet to children and a key to the success of many agritourism facilities that target families with children. With a properly designed facility, correct operating procedures, well-trained staff, and informed visitors, children can be offered the opportunity to enjoy and interact with farm animals with minimal risk. Doing it right is the best insurance policy for an agritourism facility's long-term success.
Additional resources and information:
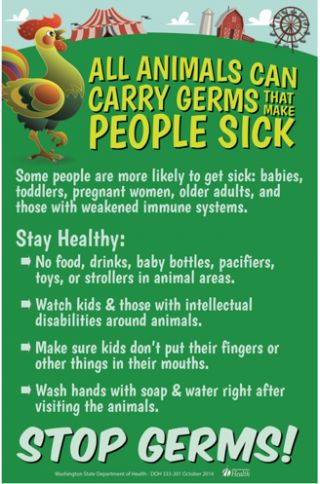
- Sample sign at the entrance to the animal area
- Sample sign at the exit of the animal area
- Sample sign at the handwashing station
- Downloadable PDFs of many type signs for animal petting areas
- National Association of State Public Health Veterinarians' Compendium of Measures to Prevent Disease Associated the Animals in Public Settings
- Safeagritourism.org has a whole series of checklists not only covering petting zoos, but also things like hayrides, corn mazes, inflatables, play areas, petting zoos, etc. They also offer walkthroughs with photos and questions followed by an explanation of the correct answer.
Subscribe to Agritourism Today